
LE QUINTREC-DONNETTE Moglie (PU-PH/UM)
BEC Nicole (IE/INSERM)
EMILIEN Thaïs (IE/CHU)
BEYZE Anaïs (MD, PhD/CHU)
CHATELAIN Juliette (MD/CHU)
SERRE Jean-Emmanuel (MD/CHU, PhD student)
kidney graft
antibody-mediated rejection
rare complement-dependent disease
recurrence of disease after renal transplantation
membranous nephropathy
immune response
endothelium
exosome
glycoengineering
transplantation mouse model
Cell biology:
Primary human endothelial cell isolation, amplification and activation; flow cytometry; immunological techniques (ELISA, CBA, IF, IHC, Western blot)
Patients cohorts (kidney biopsies, sera, urines)
Molecular biology:
RT-qPCR
Animal experimentation:
Transplantation mouse model; surgery
Our research focuses on the immunological mechanisms involved in kidney diseases, both in native kidneys and renal allografts. The group investigates key areas including allo-immunity in kidney transplantation, autoimmune renal diseases, and endothelial activation. We have developed particular expertise in studying the glycosylation of anti-HLA antibodies and its impact on endothelial cell activation, as well as the role of the alternative complement pathway and the identification of novel antigens in rare autoimmune kidney disorders. To address these questions, we combine in vitro models of endothelial and podocyte cultures with analyses of patient-derived samples, while also leveraging patient cohorts from the clinical service and developing animal models to further advance our research.
Our research axis are :
1) Allo-immunity, innate immunity and endothelial cells in renal transplantation
Our team investigates allo-immunity in kidney transplantation with a particular focus on endothelial cell responses and the role of innate immunity. We work with in vitro endothelial cell models, whose endothelial panel includes primary HUVECs (human umbilical vein endothelial cells) isolated from umbilical cords, as well as HMECs (human microvascular endothelial cells) and conditionally immortalized GECs (glomerular endothelial cells). One major project explores the biochemical properties of anti-HLA antibodies, with a specific emphasis on Fc glycosylation. Leveraging expertise in mass spectrometry and collaborations, we demonstrated that anti-HLA antibody glycosylation profiles are correlated with the occurrence of rejection, findings further supported by our in vitro models. These studies revealed new immunological mechanisms driven by distinct anti-HLA glycoforms. We are currently working on cell signaling pathways driving this new finding.
In parallel, we characterize humoral rejection phenotypes in kidney transplant recipients through spatial proteomics analyses of patient biopsies. Our overarching goal is to integrate endothelial activation, complement activation, and innate immune pathways to better understand the mechanisms underlying antibody-mediated rejection.
2) Rare kidney disease and autoimmunity in kidney diseases
The study of the alternative complement pathway represents a central focus of our research. Our group coordinates two national reference centers dedicated to rare diseases (SORARE) and thrombotic microangiopathies (CNR-MAT). We lead two national cohorts: (1) atypical hemolytic uremic syndrome and (2) recurrence of C3 glomerulopathy after kidney transplantation. In addition, we contribute to clinical development of complement inhibitors through phase I and II trials and coordinate a PHRC (Hospital Clinical Research Program) on thrombotic microangiopathy. This project aims to establish the role of MAC (C5b-9) deposits on endothelial cells as a biomarker to guide complement-targeted therapies in TMA. The assay was developed and validated by our group and the study will be completed by the end of 2025. We focused a part of the research on complement recurrence disease in kidney transplantation: understanding and complement blockers therapeutic.
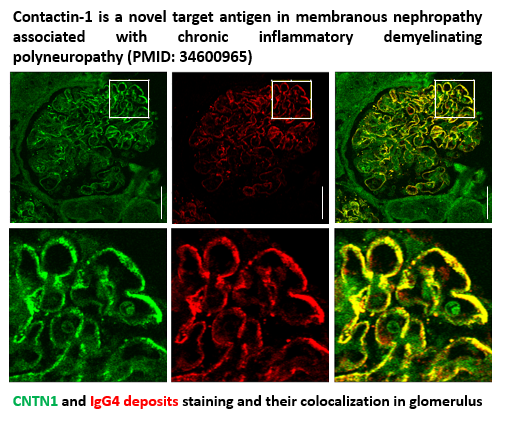
We also investigate rare autoimmune kidney diseases. We recently characterized the first neuro-renal disease association of glomerulonephritis and neurological disease, and described a shared antigen (contactin-1) between glomerular cells and nerves. In collaboration with Dr. Jérôme Devaux (neuroscience researcher at Institut de Génomique Fonctionnelle, Montpellier), we are currently developing an animal model to further elucidate the pathophysiological mechanisms underlying this association. Moreover we are working on others candidates responsible for neuro-renal syndrome.
The role of antibody glycosylation in autoimmune and alloimmune kidney diseases. Beyze A, Larroque C, Le Quintrec M. Nat Rev Nephrol. 2024 Oct;20(10):672-689. PMID: 38961307
IgG3 donor-specific antibodies with a proinflammatory glycosylation profile may be associated with the risk of antibody-mediated rejection after kidney transplantation.Pernin V, Bec N, Beyze A, Bourgeois A, Szwarc I, Champion C, Chauvin A, Rene C, Mourad G, Merville P, Visentin J, Perrochia H, Couzi L, Larroque C, Le Quintrec M.Am J Transplant. 2022 Mar;22(3):865-875. PMID: 34863025
C5b-9 Glomerular Deposits Are Associated With Poor Renal Survival in Membranous Nephropathy.Teisseyre M, Beyze A, Perrochia H, Szwarc I, Bourgeois A, Champion C, Chenine L, Serre JE, Broner J, Aglae C, Pernin V, Le Quintrec M.Kidney Int Rep. 2022 Oct 17;8(1):103-114. PMID: 36644365
Contactin-1 is a novel target antigen in membranous nephropathy associated with chronic inflammatory demyelinating polyneuropathy. Le Quintrec M, Teisseyre M, Bec N, Delmont E, Szwarc I, Perrochia H, Machet MC, Chauvin A, Mavroudakis N, Taieb G, Lanfranco L, Rigothier C, José B, Concetta C, Geneste C, Pernin V, Larroque C, Devaux J, Beyze A. Kidney Int. 2021 Dec;100(6):1240-1249. PMID: 34600965
For more references, click on PubMed